Hepatocellular carcinoma
"Any centre that seeks to be at the vanguard of hepatocarcinoma treatment must be equipped with radioembolisation, although because of its sophistication it is reasonable that there should be reference centres for this treatment".
DR. BRUNO SANGRO
COORDINATOR. LIVER AND PANCREATIC CANCER AREA

Hepatocarcinoma is the most common primary tumour of the liver. It is the fifth most common cause of cancer death in the world and, in Spain, there are between 5,000 and 8,000 new cases each year.
Today we have a wide range of treatments available: liver transplantation, resection surgery, radiofrequency ablation, chemoembolisation and radioembolisation.
In addition, in recent years, drugs have been developed that are capable of acting systemically at different stages of the disease.
The Clínica Universidad de Navarra Cancer Centre has more than twenty-five years' experience in the treatment of this tumour. Our aim is to offer the best treatment and to develop lines of research that help us to find new therapies. Our centre is at the forefront of research in this area.

A PERSONALIZED MEDICINE
Second Opinion,
peace of mind
Request a second opinion from our professionals with great experience in the diagnosis and treatment of oncological diseases
In 3 days, without leaving home.
Symptoms of hepatocarcinoma
In many cases, hepatocarcinoma does not present any symptoms until very late in its development. This is because the inside of the liver is painless and can harbour a large amount of tumour without symptoms.
Exceptionally, small tumours may cause symptoms because they obstruct the bile duct and cause jaundice, or because they rupture and cause haemorrhages.
In the event of any symptoms, the recommendation is to see a specialist.
When tumours increase in size, without causing problems, they end up causing intense tiredness, lack of appetite, unmotivated weight loss, pain under the right ribs or itching.
Do you have any of these symptoms?
If you suspect that you have any of the above symptoms,
you should consult a medical specialist for a diagnosis.
Causes of hepatocarcinoma
Hepatocarcinoma, in Spain and in the rest of the Western industrialised countries, almost always appears as a consequence of a long-standing liver disease, which in most cases is chronic hepatitis.
Most patients are over 40 years old. Hepatitis B and C viruses sometimes cause cirrhosis and some patients with cirrhosis develop liver tumours.
Cirrhosis of other origins, such as alcohol or metabolic disorders, also predispose to the development of hepatocarcinoma.
In areas where liver cancer is more common (Southeast Asia and Africa), it occurs much more frequently without the need for prior liver cirrhosis. In these regions, patients generally become ill at a younger age (before 40 years of age).
How is hepatocarcinoma diagnosed?
The Clínica Universidad de Navarra Cancer Centre performs various techniques to diagnose liver tumours, including hepatocarcinoma.
Liver elastography: innovative, bloodless, simple and fast. It improves the diagnosis and monitoring of liver fibrosis. The test takes just 15 minutes, does not require anaesthesia and is painless.
Other techniques to detect possible liver tumours include ultrasound, CT or CAT scans, MRI and liver biopsy.
Treatment of hepatocarcinoma
The aim of chemotherapy is to destroy tumour cells to shrink the disease by combining a variety of drugs, which makes them more effective.
Cancer cells grow and divide rapidly. Chemotherapy slows their growth and shows a decrease in disease relapse and an increase in survival.
The frequency and duration of chemotherapy depends on the type of cancer, the goals of treatment, the drugs to be used and how the body responds to them.
During or at the end of treatment, the oncologist will order tests to find out how the tumour responds to chemotherapy: whether it has disappeared or shrunk, whether it remains stable, or whether it has continued to progress.
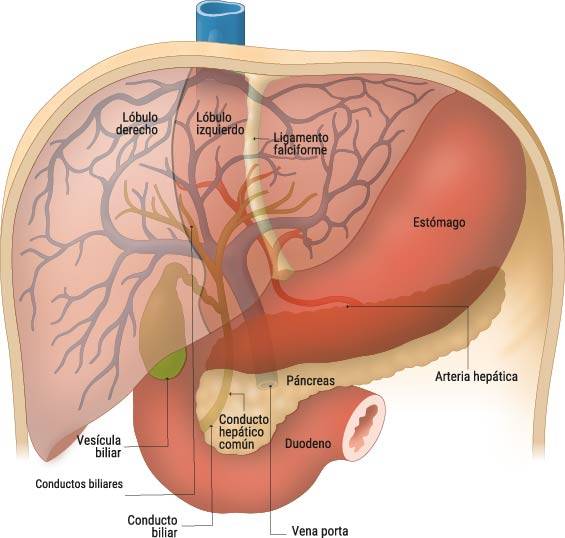
Arterial embolisation involves injecting tiny plastic spheres through the artery, as selectively as possible, to block the small vessels.
The result is that the tumour or tumours are cut off from the blood supply. The treatment is usually repeated every six weeks as many times as necessary, usually three or four times.
Although arterial embolisation does not require surgery or anaesthesia, it is common to stay in hospital for two to four days, which is necessary to control side effects such as pain, nausea and fever. Although it is not a particularly risky treatment, it is common to feel tired or have a low fever in the following days.
Embolisation is a treatment that can be used when other more effective treatments, such as surgery or radiofrequency, are not possible. Its application offers greater survival for patients and can be curative. It should be noted that it can only be used when liver function is very good.
Radiofrequency is a simple, safe and very well tolerated therapeutic technique. It is based on the application of intense heat to liver tumours, whether primary or secondary (liver metastases).
In order to transmit this intense heat to the tumours, needles are introduced into the liver through the skin, in a procedure that does not require general anaesthesia, but does require deep sedation to make it less uncomfortable. To place the needles in the tumours, the specialist is guided by ultrasound.
Once the needles are in place, the energy that generates heat is applied for a few minutes. All the tissue surrounding the needle, up to a maximum diameter of about 5 cm, is calcined. This treatment is therefore only suitable for tumours of 5 cm or less.
When tumours are not visible on ultrasound or when there are several of them and the procedure will take longer, it can be performed in the operating theatre, with open or laparoscopic surgery. In general, the hospital stay is 24 hours.
Radioembolisation with Ytrium spheresYtrium90 are radioactive microspheres that go directly into the liver. This treatment targets liver tumours and delivers millions of microscopic radioactive pellets (radium or microspheres) directly to the liver.
These microspheres contain the radioactive element Ytrium90, which radiates at a very short distance (about 2.4 mm). By placing them close to the tumour site, the radiation zone can be controlled, preventing damage to healthy areas.
Liver transplantation is the only curative treatment for serious diseases such as cirrhosis, some tumours, congenital liver abnormalities or metabolic disorders whose deficiency is in the liver. It consists of removing the diseased liver, in whole or in part, and replacing it with a healthy one from a deceased or living donor.
The Clínica Universidad de Navarra Cancer Centre has one of the best survival results: more than 90% of patients alive 1 year after the operation and an approximate survival rate at 5 and 10 years of 70 and 60%, respectively.
The team of surgeons and hepatologists at the Clínica Universidad de Navarra has performed more than 400 liver transplants, more than twenty of them from living donors. This makes the Clínica one of Spain's leading hospitals in adult living donor liver transplants.
What clinical trials do we have on hepatocarcinoma?
The Liver and Pancreatic Cancer Area
of the Cancer Center Clínica Universidad de Navarra
The Liver and Pancreas Cancer Area is a multidisciplinary area exclusively for the comprehensive approach of tumor pathology of the liver, pancreas and biliary tract, as well as living donor liver transplantation.
Patient care will be coordinated by a single reference person who is an expert in these pathologies and who will be in charge of informing and coordinating consultations, tests, treatments, surgeries, etc., in less than 48 hours.
Diseases we treat
- Pancreatic Cancer
- Bile duct cancer (Cholangiocarcinoma)
- Hepatocarcinoma or Liver Cancer
- Liver Metastases
- Other Liver Tumors

Why at the Clinica?
- Integral evaluation of the patient.
- Possibility of beginning personalized treatment 48 hours after the first consultation.
- Minimally invasive surgery for the best recovery of patients.
Our team of professionals
Learn all about cancer and its latest treatments
‘The present and future of cancer treatment is based on highly specialised teams’
Dr. Antonio González, director of the Cancer Center of the Clínica Universidad de Navarra, summarises what cancer is, causes, diagnosis, treatment and innovative advances in the future of cancer treatment.