Breast Cancer
"The survival from breast cancer has increased due to the improvement in early diagnosis and therapies applied in order to combat this pathology".
DR. ISABEL RUBIO
COORDINATOR. BREAST CANCER AREA
What is breast cancer?
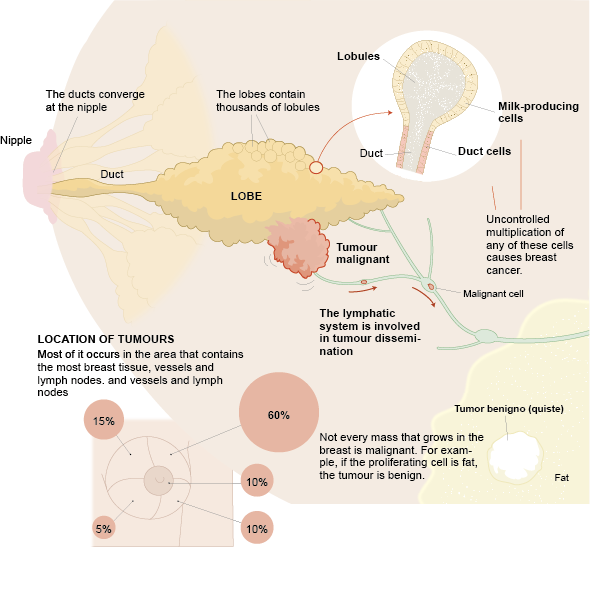
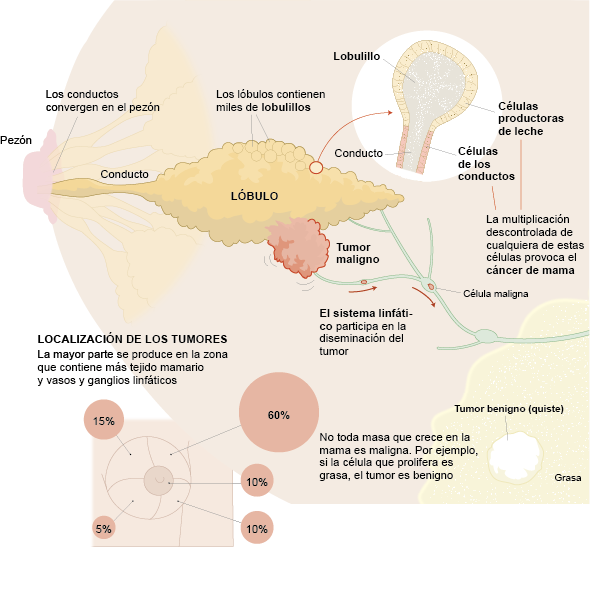
Breast cancer is a disease of the mammary gland that occurs when cells grow and multiply abnormally. As a result, they grow uncontrollably and form a tumor. It is the most common type of cancer in women, although it can also affect men.
At the Clínica Universidad de Navarra, patients who come in with symptoms are evaluated by one of our specialists and receive a personalized treatment plan that can begin just one week after completing diagnostic testing.
The Breast Cancer Area at the Clínica Universidad de Navarra is equipped with the most advanced technology for the diagnosis and treatment of breast cancer. Approximately 90–95% of breast cancer cases are sporadic. This means they are caused by changes in genes, along with other risk factors, but are not inherited.
About 5–10% of breast cancer cases are hereditary. This means they are caused by a genetic mutation that may have been passed down from either the mother or the father. At the Clínica, we will carry out the necessary tests to determine whether your cancer is sporadic (not inherited) or related to a genetic predisposition.
If needed, you will have a consultation with the Genomic Medicine Unit, where specialists in genetic counseling will clearly and thoroughly explain everything related to these genes and what they may mean for you and your family.
Contact us if you need more information or advice on the checkup you need.

What are the symptoms of breast cancer?
20% of anal cancer patients are asymptomatic. However, here are some of
the main symptoms that may be associated with anal cancer.
It is essential to see a specialist in breast pathology if you notice any of the following symptoms:
- A lump or thickened area in the breast or in the armpit (under the arm).
- Changes in the size, shape or appearance of the breast: Any asymmetry or alteration that is unusual deserves attention.
- Nipple retraction, eczema or sagging: These changes may be related to serious underlying conditions.
- Discharge of blood or other fluid from the nipple: Although not always indicative of cancer, this is a symptom that should be evaluated.
- Skin changes, such as redness, scaling or a texture reminiscent of orange peel.
- Persistent breast pain: Although breast pain is often associated with benign conditions, it can also be a sign of breast cancer.
- Partial or complete swelling of the breast, even if not accompanied by a visible lump.
Remember that early detection is key to the successful treatment of breast cancer. Seek medical attention promptly for any suspicious changes.
Do you have any of these symptoms?
If you suspect that you have any of the above symptoms,
you should consult a medical specialist for a diagnosis.
What are the causes?
The causes that produce breast cancer are multifactorial, that is, they cannot be attributed to a single factor. Among these factors are:
- Age. The risk increases with age. The highest incidence of breast cancer is between the ages of 50 and 60.
- Family history of breast cancer. Depending on the number of affected family members and their relationship, whether they are first or second degree, and the age of onset, there are different risks of developing it.
- Hereditary factors. Approximately 5-10% of cases are hereditary. Half of these cases are attributed to the mutation of two genes: BRCA1 and BRCA2. In these cases, genetic testing is recommended.
- Having your first pregnancy after the age of 30 or not having children.
- Early menstruation (before the age of 12) and late menopause (after the age of 55).
- Certain benign breast lesions, especially proliferative lesions with atypia.
- Life Style: alcohol consumption, obesity, smoking and physical inactivity.
More than half of all women with breast cancer have none of these risk factors, nor do all women with one or more risk factors go on to develop breast cancer. For this reason, early detection systems are particularly important.
What types of breast cancer are there?
There are several types of breast cancer, which are classified according to their origin (ductal or lobular), their behavior (invasive or non-invasive), and their molecular characteristics (hormone receptors and specific proteins).
95% originate in the epithelium of the mammary ducts or lobules (the tissue that internally lines the milk-transporting ducts). Depending on their location, they can be ductal, lobular or, if they affect the nipple-areola complex, they are known as Paget's disease.
Less than 1% have mesenchymal origin, that is, they come from tissues such as the connective, vascular or muscular tissues of the breast. These cases are called sarcomas, such as malignant phyllodes tumors or angiosarcoma.
The molecular characteristics of the tumor are determined by biomarkers such as estrogen, progesterone, Her2 or Ki-67 receptors. These allow the selection of personalized treatments, adapted to the characteristics of the tumor, the patient and his or her preferences. The treatment decision is always made jointly by the medical team and the patient.
Can breast cancer be inherited?
In approximately 15-20% of breast cancer cases there is a family history of the disease, with no inherited genetic mutation identified. In these cases, the risk is probably due to as yet unknown genetic factors and combination with other risk factors.
In contrast, hereditary breast cancer is caused by an identifiable genetic mutation, the BRCA1 and BRCA2 genes being the most frequent. These mutations are also associated with other types of cancer and can be passed on to offspring with a 50% probability.
Being a healthy carrier of a genetic mutation does not mean that cancer will develop, but the risk of developing cancer is significantly higher than in people without the mutation.
What is my risk of having breast cancer?
At the Clínica Universidad de Navarra, we have a Breast Cancer Risk Assessment Consultation where, after analysing the patient's family and personal history, as well as her breast characteristics, a computer programme is used to determine the approximate risk of breast cancer and recommend the most appropriate radiological tests for early diagnosis.
If you have a breast lesion that increases the risk of breast cancer, our specialists will explain the best way to follow up.
How is breast cancer diagnosed?
One of the keys to success when treating breast cancer is the comprehensive assessment by all the specialists involved in the process and the speed in establishing the best treatment guideline.
For this reason, the Clínica Universidad de Navarra has a specific medical area for the diagnosis and treatment of breast cancer, made up of a multidisciplinary team of professionals specialized in breast cancer.
A medical history and physical examination will be performed and imaging methods will be added:
- Mammography
- Breast ultrasound
- MRI or contrast mammography
- Breast biopsy - core or vacuum biopsy
How is breast cancer treated?
Breast lumpectomy
Lumpectomy or breast-conserving surgery is the surgical treatment indicated in 70-80% of breast cancer cases. It consists of removing only the tumor, preserving the rest of the breast tissue. It has been shown to have the same oncologic results as mastectomy, and also improves the quality of life of patients, according to numerous studies.
In most cases it requires a 24-hour hospital stay, although in some situations it can be performed on an outpatient basis. Whenever possible, hidden scars (such as on the edge of the areola, the submammary fold or the armpit) or oncoplastic surgery techniques, which combine oncology and plastic surgery to obtain the best aesthetic result, are chosen.
These techniques make it possible to remove the tumor with adequate margins and reshape the breast so that the aesthetic result is as good as possible, thus reducing the need for mastectomies.
In addition, survival with conservative surgery combined with radiotherapy is equivalent to that obtained with mastectomy.
At the Clínica Universidad de Navarra, our surgeons are pioneering experts in the use of intraoperative ultrasound, which improves surgical precision in non-palpable tumors and reduces the risk of positive margins.
Mastectomy
In 20-30% of cases, complete removal of the breast (mastectomy) is necessary. There are several techniques depending on the clinical case:
- Simple mastectomy: the entire breast tissue is removed, including the skin and the nipple-areola complex. It requires hospitalization for 1 to 2 days and can be combined with other treatments.
- Modified radical mastectomy: the breast tissue, the nipple-areola complex and the lymph nodes in the armpit are removed. It also requires 1-2 days of hospitalization and may include immediate reconstruction.
- Skin sparing mastectomy: the skin of the breast is preserved, but the nipple-areola complex is removed. It improves the aesthetic result in the reconstruction.
- Skin sparing mastectomy with nipple-areola complex: all the skin and the nipple-areola complex are preserved. It offers a more natural result after reconstruction. To apply it, a previous study with mammography, MRI and nipple biopsy is performed to confirm that there is no tumor involvement.
At Clinica de Navarra, we perform breast reconstruction in 90% of cases after mastectomy, ensuring a comprehensive approach that improves the quality of life and aesthetic results for our patients. In case the patient requires radiotherapy after mastectomy we also value immediate reconstruction and up to 60% of patients with subsequent radiotherapy receive immediate reconstruction.
Postoperative radiotherapy is a key step in reducing the risk of the tumor coming back in the operated area. In fact, it has been proven to reduce that risk by approximately one third.
At the Clinica Universidad de Navarra, we have extensive experience in both conventional radiotherapy (irradiating the entire breast over 6 weeks) and partial radiotherapy (irradiating only the area where the tumor was located, called the tumor bed, over just 5 days).
In cases of early-stage breast cancer, partial radiotherapy directed only at the highest-risk area offers very satisfactory results, with a minimal risk of recurrence.
The Clinica Universidad de Navarra has implemented various partial breast irradiation techniques:
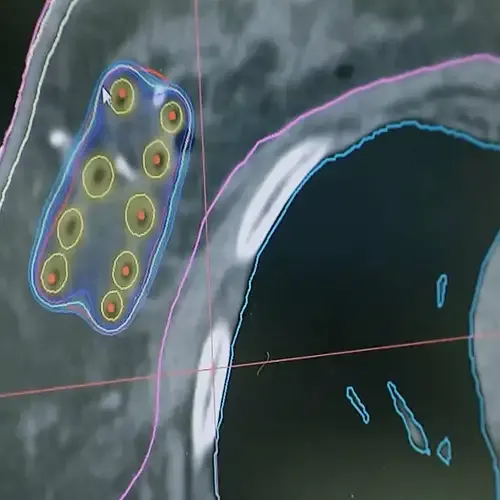
High-dose rate perioperative breast brachytherapy
- A minimally invasive procedure that delivers radiation directly to the tumor bed during the removal surgery.
- Reduces treatment duration from 6 weeks to just 5 days.
- Once completed, the catheters are easily removed in the clinic, without anesthesia.
- We are an international reference center and have the most accredited experience in this technique.
High-dose rate perioperative breast brachytherapy + external radiotherapy using the “forward” technique
- Indicated when the cancer is more widespread.
- Combines brachytherapy in the highest-risk area with external radiotherapy to the rest of the breast tissue, ensuring comprehensive treatment.
External radiotherapy using the “forward” technique
- Allows a more even distribution of radiation than the conventional technique, reducing acute side effects.
- Shortens treatment to 15 sessions, compared to the 25 sessions required in traditional radiotherapy.
Partial external radiotherapy with accelerated technique
- Irradiates only the tumor bed, without treating the entire breast.
- We use an accelerated 5-day schedule, concentrating the total dose in less time and avoiding long treatments lasting several weeks.
The choice of the most appropriate chemotherapy treatment depends on several factors:
- Tumor size.
- Involvement of the lymph nodes.
- Presence or absence of distant metastases.
- Previous treatments received.
- Breast cancer subtype (based on the presence of estrogen receptors, progesterone receptors, HER2, etc.).
- Age and overall health status.
- Other associated conditions (comorbidities).
- Possible side effects of the treatment.
In general, chemotherapy for breast cancer can be administered in three contexts:
Adjuvant (after surgery)
- Used for localized tumors to reinforce local treatment.
- Its goal is to eliminate possible tumor cells circulating in the blood or small undetected metastases, thereby reducing the risk of recurrence.
Neoadjuvant (before surgery)
- Allows systemic treatment to begin earlier.
- Helps assess whether the tumor responds to chemotherapy (if it decreases in size).
- Can reduce the tumor’s volume, making it possible to perform more conservative surgery or to operate on tumors that were initially inoperable.
In advanced or metastatic disease
- Used to control metastases and slow disease progression, improving quality of life.
At the Clinica Universidad de Navarra, we have specific protocols and extensive experience in administering chemotherapy to pregnant women with breast cancer, always ensuring maximum safety for both mother and baby.
We have a wide range of chemotherapeutic drugs available to tailor treatment to each tumor type and clinical situation.
Hormonal treatment, also called endocrine therapy, is a fundamental strategy for treating breast tumors that have hormone receptor positivity (HR+), meaning those that grow stimulated by hormones such as estrogen (ER) and/or progesterone (PR).
This type of tumor is the most common, representing 70% to 80% of all breast cancers.
In recent years, hormonal treatment for hormone-sensitive breast cancer (HR+) has evolved significantly, both in early stages and advanced disease, thanks to new medications and a more personalized approach based on the tumor’s biological characteristics.
Hormonal therapy has been proven to reduce the risk of recurrence and improve survival in patients with this type of cancer.
Selective Estrogen Receptor Modulators (SERMs)
- Example: Tamoxifen.
- Blocks the action of estrogen in tumor cells, preventing their growth.
Aromatase Inhibitors
- Examples: Anastrozole, Letrozole, Exemestane.
- Reduce the amount of estrogen produced in the body, thereby limiting hormonal stimulation of the tumor.
LHRH Analogs (luteinizing hormone-releasing hormone)
- Examples: Goserelin, Triptorelin.
- Block estrogen production in the ovaries, being especially useful in premenopausal women.
SERDs (Selective Estrogen Receptor Degraders)
- Examples: Fulvestrant, Camizestrant, Elacestrant.
- Not only block the action of estrogen but also destroy the estrogen receptor in the tumor cell.
- Currently approved for advanced or metastatic breast cancer and under study for early-stage disease.
Other associated drugs: CDK4/6 Inhibitors
- Examples: Palbociclib, Ribociclib, Abemaciclib.
- Used in tumors with hormone receptor positivity and HER2 negativity, in advanced or metastatic disease.
- CDK4 and CDK6 are proteins that regulate the cell cycle, meaning the process by which cells grow and divide.
- These drugs block that cell division and are usually administered along with hormonal therapy such as letrozole, anastrozole, fulvestrant, or tamoxifen.
- They have represented a major advance in treatment, prolonging disease control.
The immune system plays a key role in defending against cancer. Immunotherapy aims to stimulate or “retrain” the patient’s natural defenses so that her own body can recognize and attack the tumor cells.
In breast cancer, immunotherapy has gained an important role, especially in aggressive subtypes such as triple-negative breast cancer (TNBC), which lacks hormone receptors and HER2, and for which conventional treatment options are more limited.
How it works
One of the most commonly used strategies is immune checkpoint inhibitors (anti–PD-1 and anti–PD-L1 antibodies).
- These drugs work by “releasing the brakes” on the immune system, allowing the body’s defenses to attack the tumor more effectively.
- In combination with chemotherapy, they have been shown to improve survival and disease control in patients with advanced or metastatic breast cancer.
Personalized breast cancer vaccines
At the Clinica Universidad de Navarra, personalized vaccines are also used within immunotherapy protocols:
- They are made from the patient’s own cells (autologous vaccines), avoiding the risk of rejection.
- Tumor antigens (unique markers) are obtained so that the immune system can identify and attack the cancer.
- They are administered together with chemotherapy, especially in cases of localized disease that require this treatment.
Advantages
- Good tolerance, since it is a product derived from the patient’s own body.
- Individualized treatment that is compatible with chemotherapy.
- Can be maintained for a prolonged period, especially during the first 5 years after diagnosis, when the risk of recurrence is highest.
How they are produced
- Cells are collected from the patient and processed in the Clinica’s GMP Cell Therapy Laboratory.
- From them, the tumor antigens are extracted and incorporated into the vaccine.
- The treatment is administered according to a two-year vaccination schedule as a complement to the standard oncology treatment.
Research and current use
The Clinica has conducted a clinical trial to evaluate the effectiveness of these vaccines in a subgroup of breast cancer patients without HER2 protein expression.
They are currently offered as compassionate use therapy to complement standard treatments.
In some cases of breast cancer, tumor cells produce an excess of a protein called HER2 (human epidermal growth factor receptor 2). This protein stimulates the tumor to grow more quickly and aggressively.
Approximately 10% to 20% of breast cancers show this overexpression of HER2.
For this type of tumor, there are specific treatments with HER2 receptor inhibitors that have proven to be highly effective when combined with chemotherapy, achieving:
- Greater tumor response to treatment.
- Longer survival.
At the Clinica Universidad de Navarra, we continue to research new therapies aimed at increasing efficacy and reducing the side effects of these treatments.
Antibody-Drug Conjugates (ADCs)
ADCs (Antibody-Drug Conjugates) are one of the most innovative strategies for treating breast cancer, especially in HER2-positive or triple-negative tumors.
How they work:
- They combine a monoclonal antibody (which recognizes a specific protein on the tumor cell, such as HER2 or Trop-2) with a highly potent chemotherapy drug.
- The antibody acts like a “guided missile,” binding only to cancer cells that express that protein.
- Once bound, it releases the drug directly inside the tumor, destroying malignant cells and reducing damage to healthy tissues.
Advantages:
- Greater precision in targeting the tumor.
- Less overall toxicity than conventional chemotherapy.
- Proven improvements in survival and quality of life in patients with advanced or metastatic breast cancer.
Currently, there are ADCs already approved for the treatment of breast cancer, and many others are in advanced stages of research.

A PERSONALIZED MEDICINE
Second Opinion,
peace of mind
Request a second opinion from our professionals with great experience in the diagnosis and treatment of oncological diseases
In 3 days, without leaving home.
Or if you prefer you can come to the Clinica.
Why choose the Clínica Universidad de Navarra
THE MOST AVANT-GARDE TREATMENTS

Oncoplastic surgery and
Breast reconstruction
Our surgeons specialize in surgical planning to preserve as much healthy breast tissue as possible and, if necessary, to carry out immediate breast reconstruction.
- Conservative oncoplastic surgery.
- Nipple–areola-preserving mastectomy.
- Intraoperative ultrasound.
- Prevention of axillar lymph node involvement.
- Immediate breast reconstruction.
Targeted therapies and immunotherapy for breast cancer
We have extensive experience in administering the most innovative therapies, such as vaccines based on dendritic cells, which complement standard treatments.
- Immunotherapy-based treatments.
- Breast cancer vaccines.
Accelerated partial breast irradiation
We are pioneers in Spain in accelerated partial breast irradiation with brachytherapy, reducing radiotherapy courses to five days instead of the standard twenty-five days.
- Interstitial brachytherapy.
- Intraoperative brachytherapy.
- Intraoperative radiotherapy.
- Innovative radiotherapy techniques (proton therapy).
Proton therapy for cancer
Proton therapy is the most precise external radiotherapy modality, providing better distribution of radiation dose and therefore less irradiation of healthy tissues.
The Proton Therapy Unit of the Cancer Center Clínica Universidad de Navarra in its Madrid headquarters is the most advanced in Europe and the first in a Cancer Center, with all its healthcare, academic and research support.
Nuestro equipo de profesionales
We help our patients to overcome their stories
Their testimonies encourage us to continue improving our services